 |
| Black spider monkey |
Counting beans
Remember when Donald Trump said in June 2020, to universal derision, “If we stop testing right now, we'd have very few cases, if any”?
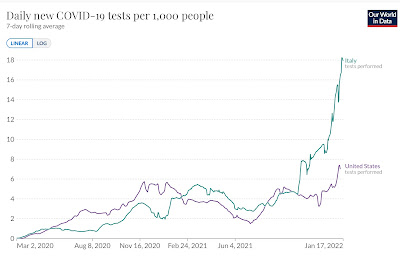
Joe Biden’s US seems to be following Trump’s advice. Take a look at the first graph above: Italy is running 35-40% more cases per capita than the United States. When I first saw such a graph I was flummoxed – how could the Italians be doing worse, when far more of them are vaccinated, almost twice as many are boosted, vaccine passports are enforced, and everyone wears masks indoors. Then I looked at the lower graph, and the reason became clear: Italy is doing nearly 3 times as many tests per capita. Seek and ye shall find. No seek, no find.
I might mention that despite frequent declarations in the US that testing “in Europe” is free or costs only pennies, Italians shell out €15, about $18, every time they do an antigen test in a pharmacy.
The Biden administration’s current party line can be interpreted as: it doesn’t really matter how many people get sick. As per Anthony Fauci: “it is much more relevant to focus on the hospitalizations as opposed to the total number of cases.” This while experts such as Eric Topol emphasize that even the awful official statistics vastly undertimate the true state of the pandemic, with many “colds” and “flus” actually being COVID-19. (By the way, the US has one-third more hospitalized COVID-19 patients per capita than Italy.)
Scope of the problem
 |
| Long COVID clinic Policlinico Gemelli, Rome |
After that prelude, on to my real subject: an update on long COVID. It’s probably the biggest reason case numbers count, and is why I myself do everything within my power to avoid getting infected. If Omicron is sooner or later going to infect “just about everybody” or even just “more than 50%,” how many will develop long COVID? So far, of course, we have no idea, the variant having arrived on the scene less than 2 months ago. We can hope that being milder Omicron will cause fewer cases, but even the mildest cases of COVID-19 can bring prolonged symptoms, so we could be in for an overwhelming secondary pandemic.
Definitions: The World Health Organization convened 265 experts from more than 30 countries, many of them long-haulers themselvers, to use the “Delphi consensus method” to develop a definition. Here’s the short version: “Post-COVID-19 condition occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset, with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis.” Another careful study laid out various subtypes, using a superb data set the authors continue to mine for more information.
Numbers: If anything they’ve become bleaker as time goes by. One recent review and meta-analysis found that a third of COVID-19 patients still suffered from fatigue 6 months after their illness, with fully half of the women complaining of brain fog. Another review concluded that more than half of COVID-19 survivors still had at least one COVID-related symptom 6 months later. A third estimated that 43% of all cases diagnosed worldwide have or have had long COVID, meaning about 100 million long COVID cases when they wrote, and more than 134 million now. Vaccination, contrary to early optimism, seems to reduce the risk only by half, according to studies of healthcare workers in Israel and app users in the UK.
Severity: The WHO panel said gently that the symptoms “generally have an impact on everyday functioning.” To get an idea of what that really means, I strongly suggest checking out this article about physician-patients, and this oneabout regular folks.
Light at the end of the tunnel?
 |
| Microclots circulating in the blood |
 |
| SARS-CoV-2 viral particles in thyroid, esophagus, spleen, and colon |
Overviews of long COVID in journals such as Science and The Lancet have concluded that the condition is basically untreatable, that all we can offer is analgesics for pain, breathing exercises for faintness, and modest advice for fatigue and shortness of breath. The one thing that has led to striking improvement in some patients is a dose of SARS-CoV-2 vaccine, as reported anecdotally and confirmed by one large international poll. Vaccination makes some patients worse, though, and we have no way of predicting which way an individual patient will react.
In the last few months, though, there may finally be some progress in understanding both what causes long COVID and how it could be treated. Theories vary but overlap to some extent, and I’ll attempt to present them in a logical order:
Tissue damage: Severe COVID-19 can damage the lungs and the heart, leading to long-lasting organ dysfunction that would explain some prolonged symptoms. Many long COVID sufferers were never severely ill, though, and a considerable proportion have no readily demonstrable organ dysfunction.
Blood clots: The South African scientist Etheresia Pretorius believes the secret of long COVID is tiny inflamed clotsthat plug up the circulatory system and inhibit the transport of oxygen to tissues. She admits that affected patients have no obvious signs of persistent clotting or inflammation, but thinks their blood is carrying inflammatory molecules and auto-antibodies sequestered inside fibrin amyloid microclots that can be detected only using special, highly refined techniques. In possible support of this theory, one small series found that a majority of long COVID patients with “brain fog” had technitium (Tc-99m) brain scans that appeared to show reduced blood flow. The clot theory would, of course, imply that long COVID could be treated using antiplatelet drugs and/or anticoagulants. Dr. Pretorius and her colleagues tried just such a combination, in a tiny number of cases, producing a manuscript claiming that 24 out of 24 patients found their symptoms not just improved by cured by such treatment! These were not unselected long COVID patients, though, but a less-than-well-defined subgroup of a 845-patient database. This seems too good to be true, and since anticoagulation is potentially dangerous I wouldn’t leap to try it; we’ll know more if and when a planned large controlled trial comes off.
Inflammation: Ordinary markers of inflammation such as C-reactive protein are sometimes but not always found in the blood of long COVID patients, and such patients often had particularly low levels of such markers during their acute phase. Some think nonetheless that inflammation underlies the condition and have turned to the prototypical antiinflammatory drugs, corticosteroids, as treatment. In a tiny case series in Madrid, 9 out of 9 long COVID patients had shifts in the subpopulations of some white blood cells (lymphocytes and monocytes) in a pro-inflammatory direction. The researchers tried giving these patients an extremely brief course of steroids, lasting only 4 days, and say that nearly all their symptoms resolved. Again, this seems too good to be true, and, again, a proper controlled trial is said to be in the works.
Autoimmunity: Patients with severe COVID-19 frequently develop autoantibodies against normal body tissues, and these often persist in long COVID. One study found long-lasting autoantibodies more common in women following asymptomatic infections, and in men after symptomatic COVID-19, with specific patterns of antibodies also varying by gender. Corticosteroids are a mainstay of treatment for autoimmune diseases such as lupus, so this is yet another line of thinking that would suggest steroids might help long COVID. Some long-hauler clinics do prescribe low-dose steroids to patients on empirical grounds, but I’ve been unable to find trials even in a planning phase.
Abnormal immune response: Researchers in London identified distinctive patterns of T cells in patients with long COVID that led them to prescribe combined histamine blockade (famotidine plus fexofenadine) to 49 patients, and they have reported that 35 of them improved. Antihistamines have become part of the large-scale Stimulate-ICP studyfrom University College London, so we should have some better evidence in a few months. But these drugs are harmless enough that I have already tried prescribing them. Anomalous immune responses – goosing the immune system – might contribute to explaining post-vaccine improvement.
Blunted immune response: Case series in Spain and Belgium have reported that patients destined for long COVID have not just low inflammatory markers but also weak antibody responses at the time of their original infection. I have also heard anecdotally that many long COVID patients produce few antibodies after vaccination. This poor immune response may make it harder to clear the coronavirus from the body, allowing it to continue at length both causing direct damage and stimulating the immune system. The virus does not keep shedding from the nose, though, so long COVID patients are not contagious.
Live virus: …and we now have another, very different kind of evidence that the virus itself may hang around at length. National Institutes of Health researchers performed autopsies on 44 patients who died weeks or months after being diagnosed with COVID-19 by PCR-swabs, looking for viable coronavirus in body tissues. Their prepublished manuscript says they detected SARS-CoV-2 in all 44 cases, scattered through tissues including not only the lung as expected, but also heart, brain, kidney, lymph node, muscle, thyroid, even testicle and ovary. Most of these patients had died within days from raging COVID-19, and in them the presence of live virus is not surprising. But 7 of them died much later, as many as 7 months after the acute illness. These findings are both novel and surprising, since the virus has always been thought to disappear quickly unless the patient had AIDS or was otherwise immunosuppressed. None of these autopsied patients were known to have long COVID, but to me the findings imply the exciting suggestion that antiviral drugs such as Paxlovid could conceivably be useful in treatment.


No comments:
Post a Comment