No, COVID-19 is not worse if you get it twice! Also lots about vaccines and long COVID, quick updates on variants and the state of the pandemic, plus extras on masks, Paxlovid, Rochelle Walensky, and one small but egregious conspiracy theory.
Treatment news
Monoclonal antibodies: The CDC has thrown cold water on the modest optimism I expressed in my last post, by saying BQ.1 and BQ.1.1 are likely resistant to bebtelovimab, and also, with BA.4.6, BA.2.75.2, and BF.7, to Evusheld. Arggggggh! In mid-November BQ.1 and BQ.1.1 officially overtook BA.5 in the US.
Paxlovid triumphs: We’ve long hoped that antiviral treatment might reduce the risk of long COVID. Now a large study from the US Veterans Administration, available as a preprint, says yes, reporting that antiviral treatment reduced by 26% the risk of still having symptoms at 90 days. Two caveats. One: VA patients are mostly elderly men, whereas long COVID mostly strikes middle-aged women. The other: diagnoses were made by chart review, without interviews or even questionnaires. Charts are great at detecting heart disease, pulmonary embolism, etc., but they’re unlikely to record such core long COVID symptoms as fatigue, shortness of breath, and brain fog. Nonetheless, I will change my clinical practice on the basis of this study. Until now I have advised older patients with mild, rapidly-improving COVID-19 symptoms that they can skip Paxlovid. Now I will start saying take it.
Molnupiravir hits the skids: Remember Merck’s antiviral? The one that (as per my own Letter to the Editor) didn’t even work on Delta, much less Omicron? People feared its use might breed new, resistant variants. Now it seems that is probably starting to happen.
Second acts
We’ve seen ample evidence that COVID-19 is milder the second time around, as summarized in a pre-Omicron literature review. An Italian study before variants emerged and a slightly later Qatari study both found repeat infections fully 90% less likely to result in hospitalization or death. And an American study of Emergency Room patients said second bouts entailed lower risks of pneumonia, heart failure, and kidney damage.
But now a massive study from the US Veterans Administration seems to say exactly the opposite: repeat attacks of COVID-19 are more severe, for both acute outcomes and long COVID. Particularly puzzling since the study extends well into the period of dominance of the milder Omicron variant. News outlets immediately blasted headlines such as “Repeat COVID is riskier than first infection, study finds” and “Each SARS-CoV-2 reinfection causes more severe disease.” The authors themselves have fed the flames. HOWEVER: they’re all dead wrong, and the contradiction with earlier studies is only apparent. That’s because the VA paper did not compare people with reinfection to those without reinfection. It was based on a database of medical records, so it could include only people sick enough to have required medical attention, which especially in the Omicron era is a small minority. As Jeremy Faust points out, the only lesson to draw is “repeat coronavirus infections are not good, especially for older people who are likely to have existing medical problems (i.e., Veterans Administration patients). This is not exactly breaking news.”
Vaccine and prevention news
Bivalents in the lab: Research results are mixed. One New York group reported that the bivalent BA.4/5 Pfizer and Moderna boosters induced no more neutralizing antibodies against Omicron BA.5 than a 4th dose of the original monovalent vaccine. Researchers from Boston did find modest antibody superiority for bivalent BA.5 boosters, but no better than for bivalent BA.1 vaccines. Moderna says its BA.1 bivalent booster induced 75% more anti-Omicron neutralizing antibodies than the original monovalent booster, but this advantage did not translate into protection against infection or clinical COVID-19. Moderna also claims its bivalent boosters induce a “robust” neutralizing antibody response against BQ.1.1, but the titres they report look minimal to me. Pfizer and BioNTech now say anti-BA.4/5 neutralizing antibodies rose 4 times higher after the BA.4/5 bivalent vaccine than after their monovalent booster, without reporting real-world outcomes.
Bivalents vs. monovalents in the real world: Among Israeli healthcare workers, a fourth dose of the original monovalent Pfizer vaccine boosted protection against Omicron infection substantially, but only for 3 months. And we finally have some concrete evidence in favor of bivalent vaccines, in the form of a very recent CDC study. Twenty-four percent of people with positive PCR swabs were unvaccinated, 72% had received 2-4 doses of monovalent vaccines, and 5% had received a bivalent booster. Among vaccinated patients, the added protection from the bivalent booster varied according the time since a person’s latest monovalent dose. When the last monovalent dose was just 2-3 months earlier, the bivalent booster increased protection against infection by about 30%. But when it had been 8 months earlier and had likely worn off, the added protection was 43%-56%. This does show that bivalent boosters increase protection against COVID-19 above and beyond the effect of previous vaccination. It does not tell us whether another dose of the original monovalent vaccine might have done the same, or what the effect is on new-entry variantssuch as BQ.1 and XBB, or how long the boost will last, given that the bivalent boosters – given an average of 4 weeks earlier – were at their peak.
Brass tacks: As of mid-October the World Health Organization was agnostic, saying the data did not support using bivalent vaccine boosters rather than ancestral-virus-only boosters. Bottom line: if you’re at increased risk, because of age or otherwise, get a booster now, ahead of any winter surge. It probably makes little difference which one.
Beta boosters: European makers Sanofi-GSK have thrown their hat in the ring with a monovalent booster, “VidPrevtyn Beta,” based on the Beta (South African) spike protein. It produced 2.5 times more Omicron BA.1 and BA.4/5 neutralizing antibodies than did a third dose of Pfizer, and has already been approved by the European Medicines Agency. We’ll see whether it catches on.
Sniffed: People have dreamed of alternative vaccine routes for a long time now, thinking that oral or nasal vaccines could be more effective than injections, by increasing IgA “mucosal” antibodies and possibly better stimulating T-cell immunity. Now an intranasal vaccine booster using the spike protein has been shown to be effective – in mice – against multiple SARS-CoV-2 strains. Eric Topol goes so far as to say, “This is the variant-proof booster we need now to help prevent infections & spread.” Lets hope so, with the caveat that mice aren’t men. Unfortunately the resistance of congressional Republicans to authorizing further pandemic spending means work on American mucosal vaccines is likely to proceed not at warp speed but at a snail’s pace. And in a bizarre twist, Pfizer seems to prefer to throw tens of millions of leftover doses down the drain rather than allow a few of them to be used for research; Moderna has been marginally more cooperative.
Puffed: The Chinese company CanSino created an injectable viral vector COVID-19 vaccine barely efficacious enough to meet World Health Organization criteria. Now it’s developed an inhaled version that will soon be offered as a booster in several Chinese cities, delivered using a device vaguely resembling an overgrown asthma inhaler. It is said to elicit somewhat more Omicron BA.1 neutralizing antibodies than Sinovac – a low bar – but in the absence of even a preprinted manuscript it’s not clear whether the antibodies fade rapidly or persist for more than 6 months.
Mix-and-match immunity: A study of California state prison inmates has found that Delta-variant infection and three-dose vaccination each gave approximately 40% protection against infection (or reinfection) in the early Omicron period – with a combination of infection plus triple vaccination lowering risk by nearly 85%. Pre-Delta infections were somewhat less protective, and mere double vaccination much less protective. The researchers also present results among prison staff, but I find them uninterpretable.
Children: A study from Qatar confirms that 2 doses of a Pfizer vaccine do very little to prevent Omicron infection. In school-age children a peak of 50% effectiveness fell to practically nil by 3 months, with even less protection in older, larger kids (Pfizer for kids is a fixed low dose). The primary series worked a bit better in adolescents, who received the 30-mcg adult dose, and lasted somewhat longer. The modest, brief effect against Omicron is confirmed by an American study – which did find that one Omicron infection was very protective against a second one, and that, as usual, vaccination plus infection is even better.
The global South: The World Health Organization has chosen to see the glass half-full, emphasizing the progress that’s been made against the pandemic. But only 20% of people in low-income countries have received a primary vaccine course, versus 75% in high-income countries. That’s triple where we were at the beginning of March, but still. Note that this February South African scientists announced that they had succeeded in replicating Moderna’s COVID-19 vaccine. But 9 months later, they’re saying it will be yet another 18 months before their product becomes commercially available. What value will it have then? Moderna immediately sued to block the project and, it seems, is still trying.
Exercise: A review article concludes that regular physical activity reduces the risk of SARS-CoV-2 infection slightly, the risk of severe disease by a third, and the risk of death by an astonishing 43%. Eyeballing their Figure 3, I’d guess those benefits only kick in at around 2 hours a week of moderate-intensity aerobic exercise.
Iron men, iron women
Some people intensely exposed to COVID-19 never catch it themselves. They seem to be rare birds in the Omicron era, with my friends and patients generally saying not “I got COVID,” but “We got COVID.” But a CDC study from this spring showed that only half of people living in the same home as a COVID-19 case ever caught the infection, and that even in households where the patient wasn’t isolated and didn’t wear a mask that rate only reached two-thirds. As you see from the graphic, the CDC emphasized the downside of those findings. But what I find amazing is on the contrary how many of those intimate contacts stayed well.
The state of the pandemic
Just while the term “post-pandemic” is being bandied about, most experts (though not all) are asking not whether we’re in store for a winter surge, but just how bad it will be. It’s already hit in Italy, where the number of confirmed cases has quadrupled in the last month, and the number of deaths has nearly doubled, with one in 5 cases a reinfection. Here, for Italian speakers, is a detailed report.
In the US the official number of new cases has remained stable, at around one-fifth Italy’s rate per capita. Deaths, however, are running neck and neck. What that suggests is that most infected Americans aren’t reporting their positive home tests to the authorities. As of this week more than 60% of US cases are caused by BQ.1 and BQ.1.1, but in Italy, the latest stats say 2/3 of cases are still BA.5, 1/3 BQ.1.
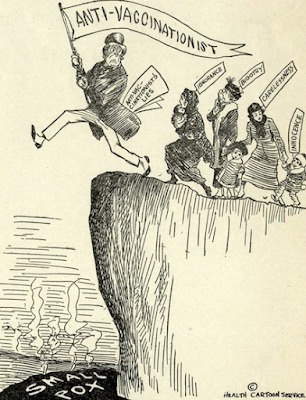
Black Americans used to die disproportionately from COVID-19, but now the tide has turned, with whites 40% morelikely to die. The reason? Vaccine hesitancy. Though once higher percentages were found among blacks, diehard novaxxers are now much more likely to be Trumpy whites. And though most deaths now occur among the vaccinated, vaccine holdouts are 5 times as likely to die of COVID-19 as someone who’s fully vaccinated, and 10 times as likely as someone with two boosters. (Thanks to Lisa Paglin and Marianna Brilla for the 1924 cartoon.)
The United States saw more deaths per capita last winter than any other large wealthy country: twice as many as Italy, 3 times as many as Canada, more than 10 times as many as Japan. Mortality was lowest in states with high vaccination rates, but even there it surpassed other countries.’ The reason is probably that the US has lagged in giving the boostersso crucial for combatting Omicron.
Back to basics
Hard evidence about masking is scarce, and now that everybody has been going barefaced a new New England Journal of Medicine article is very timely. Lifting of mask mandates in some but not all Massachusetts school districts provided a neat natural experiment, with clear results. Districts where masking was made optional had 44.9 more cases per 1000 students and staff than districts where it remained obligatory, which nearly doubled the case rate, even though schools that kept mandates had worse physical condition, more low-income students, and more crowded classrooms. Students had 39.9 excess cases per 1000, while staff, who as adults risked more, had 81.7. Though I strongly favor indoor masking I was somewhat surprised at these results, since data have suggested that kids with COVID-19 usually catch the infection not in the classroom but at friends’ homes.
Variant watch
Twelve months into the Omicron era its descendants are breeding like rabbits. No sooner had BQ.1 and BQ.1.1 appeared on the scene when XBB popped up, apparently even more transmissible and resistant to antibodies. It’s a chimeric blend of BA.2.10.1 and BA.2.75, whose latest subsubvariants include CH.1 and CH.1.1. In early October XBB was only causing about 1.3% of new cases globally. Despite claims on social media, there is no evidence it is more severe than other Omicron subvariants. For everything there is to know about Aeterna, Gryphon, Mimas, Pisces, and more see one review article from October 3rd, and another from October 31st that claimed 390 Omicron subvariants and 48 “recombinants.” Five weeks later, even that second article is likely outdated.
Dragging on
Numbers
Estimates of the rate of long COVID vary wildly. One pooled analysis said 6.2% of COVID-19 patients still had symptoms at 3 months, using a relatively narrow definition. A modelling study from the World Health Organization similarly estimated 17 million long COVID cases in Europe in 2020-21, about 7.1%. The US government calculated that 7.7-23 million Americans had long COVID in February 2022.
A large Scottish study, however, reported that 42% of COVID-19 patients still had symptoms 6-18 months after their bout. And in a smaller study by Spanish researchers who got a particularly high number of invitees to cooperate, 59.7% of hospitalized patients and a shocking 67.5% of outpatients had at least one residual symptom 2 years after their acute infection, primarily pain, fatigue, and cognitive impairment. Similar to a Chinese study finding that 55% were still not completely well after 2 years. One major caveat: most of the patients in all 3 studies were infected with the original Wuhan strain of SARS-CoV-2, before the arrival of vaccines, antivirals, or Omicron.
We’ve hoped Omicron patients would be much less prone to long COVID. But according to official UK government analyses the percentage of people with persistent symptoms 12 weeks after Omicron is only 10-15% lower than after Delta, among people who are triple-vaccinated. The rate was halved, though, among people who’d had only two doses of vaccine.
Symptoms
The manifestations of long COVID can apparently include both low semen quality and erectile dysfunction. I believe it, partly because so many women have told me they lost their libido when they had COVID-19.
In older people, COVID-19 increases the risk of both dementia and Parkinson’s, with a 69% increase in new diagnoses of Alzheimer’s disease during the year after infection. The Alzheimer article’s co-author Dr. Pamela Davis hypothesizes at a physicians-only website that “persons who already had declining cognitive function were tipped over into frank Alzheimer's disease.” Another reason for us older people to do everything we can to avoid catching COVID-19 (we all have some degree of declining cognitive function). A giant study by the Alzheimer's Association Global Consortium should eventually shed more light.
Causes
The South African researcher Etheresia Pretorius has published a paper confirming her previous observations of abnormal clotting phenomena in the blood of long COVID patients, in the form of hyperactivated platelets and microclots of fibrin/amyloid.
I’m a believer, given the evidence of impaired circulation in the lungs, hearts, and brains of long COVID patients. But, with others, I confess to finding it odd that nobody except Dr. Pretorius ever seems to detect those microclots, and slightly suspicious that she’s apparently hypothesized the same underlying mechanism for diseases from diabetes to lupus and Parkinson’s. And I’d like to see better evidence that treatment attacking the clots works than the pilot studyDr. Pretorius reported a year ago. Fortunately that evidence may arrive soon: the British STIMULATE-ICP trial testing other treatments the anticoagulant rivaroxaban (that might dissolve microclots) finally began enrolling patients this summer.
MRI brain scans on 15 post-COVID-19 patients showed mild abnormalities that could have been vascular, though there was little difference between patients with and without fatigue or brain fog. More to the point is a study that using a “susceptibility-weighted” MRI demonstrated post-COVID-19 abnormalities in the frontal lobe and brain stem, brain regions linked with fatigue, insomnia, anxiety, depression, headaches and cognitive problems. The researchers’ press release hinted that some of their subjects had long COVID but unfortunately didn’t compare that subgroup with others. Other post-COVID changes include poor circulation to the heart muscle and fibrotic scarring of the lungs (especially relevant to patients from early in the pandemic).
Prevention
Vaccination may help protect against long COVID when people get breakthrough infections. Studies among general populations have given vaccinees variously a 15% (US), 28% (Scotland), and 50% (UK) advantage over the unvaccinated. The authors of one systematic review concluded that vaccination helps but declined to quantify how much. A preprinted study of 280 chronic rheumatological disease patients, however, has found those who were fully vaccinated to be only one-tenth as likely to have persistent symptoms 3 months after a breakthrough infection. Since no previous study has found such a strong protective effect, it might be specific to patients with autoimmune conditions. But, as always, the best way to avoid getting long COVID is to avoid getting COVID-19 in the first place, so keep up to date with your boosters.
…As I’ve said treatment with Paxlovid seems to cut risk somewhat.
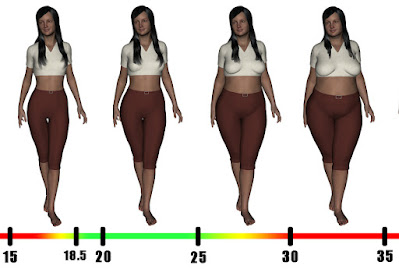
And so may – surprisingly – weight loss. A new British study found that every additional point of Body Mass Index (weight squared in kilograms divided by height in centimeters), increases the risk of long COVID by 2.7%. That means that all other things being equal someone who barely qualifies as obese (BMI = 30), is 22% more likely to develop long COVID than someone in the middle of the normal range (BMI = 22), and someone morbidly obese (BMI = 40), like 11.5% of American women, runs a 50% higher risk.
Treatment
No news. The Washington Post describes desperate long COVID sufferers turning to charlatans who peddle everything from ivermectin to earthworm extract. Unfortunately when it came to hyperbaric oxygen treatment this otherwise excellent article got it wrong. They linked to a year-old pilot study – 10 patients who said they felt better after treatment than before – but ignored the excellent research published this summer that demonstrated marked improvement with HBOT as compared with a sham control treatment.
Rachel, Rachel, I’ve been thinking
OK, so Rochelle Walensky, the head of the CDC, has had COVID-19. No scandal there, though as per the photograph above, she hasn’t always been superprudent. And – like Anthony Fauci and Joe Biden – she had a relapse of symptoms and test positivity a few days after finishing a course of Paxlovid. Clearly this phenomenon is much more common than Pfizer admits. BUT: unlike Fauci and Biden, she had no business taking Paxlovid in the first place. They are both far over 65, the cutoff after which Palovid definitely helps avoid hospitalization and death. Walensky is in her 50’s, even younger than Kamala Harris who was given Paxlovid even more scandalously, for an asymptomatic infection, where it is never indicated. If I myself know that Paxlovid does little or nothing for people under 65, even those at high risk because of chronic disease, I’d expect that Walensky to know so as well. And if I know that Paxlovid, while reducing risk of hospitalization, doesn't relieve symptoms, Walensky should be at least as well-informed.
Have they no shame?
This unfortunate child was actually not connected with the COVID vaccination campaign in any way, and his death from pneumonia was in no way related to either COVID-19 or COVID-19 vaccines.